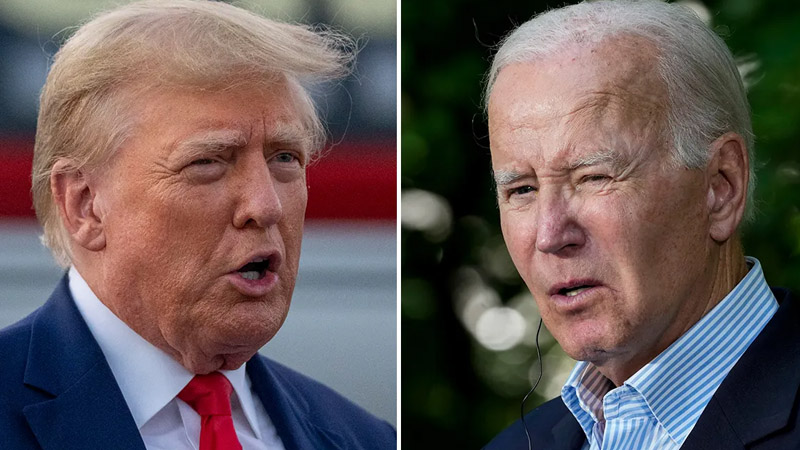
Just as the Biden administration appeared poised to broaden Medicare access to popular weight-loss drugs like Ozempic and Wegovy, the Trump administration swiftly halted the effort. On Friday, April 4, President Donald Trump’s team formally shut down the proposed plan in a sweeping 438-page regulatory update, signaling its resistance to Biden’s billion-dollar bet on anti-obesity medications.
Back in November, the Biden administration unveiled a bold strategy aimed at sidestepping a decades-old rule that prohibits Medicare’s Part D from covering weight-loss treatments. The proposed change sought to expand coverage to include drugs initially designed to treat diabetes but now widely used for weight management. The rationale, Biden officials argued, was rooted in public health, not vanity.
More: Laura Loomer Sparks Firings at NSC After Oval Office Meeting
More: Trump Sparks Outrage for Skipping Ceremony Honoring Fallen Soldiers to Attend Saudi-Backed Golf Event Instead
These medications, including Ozempic and Wegovy, were championed by the administration as critical tools for treating obesity and its dangerous side effects—such as heart disease, diabetes, and sleep apnea. If the plan had passed, an estimated 3.4 million Americans could have gained access through Medicare and Medicaid programs, The New York Times reported.
But the projected cost was staggering: $35 billion over the next decade, or roughly $3.5 billion annually. That kind of price tag drew scrutiny from the Department of Government Efficiency (DOGE), a newly formed agency under the Trump administration tasked with eliminating what it calls “wasteful” federal spending.

The Trump administration’s decision came without a detailed explanation. Instead, the final regulation offered a polite and vague dismissal. Catherine Howden, spokesperson for the Centers for Medicare and Medicaid Services (CMS), said in an email, “The agency believes expanding coverage just ‘is not appropriate at this time.'” However, she added that CMS “may consider future policy options.”
Currently, Medicare does offer coverage for these medications, but only under limited conditions, such as for individuals diagnosed with diabetes or obesity-related illnesses like cardiovascular disease or sleep apnea. Biden’s plan would have removed those restrictions, granting broader access without the need for secondary diagnoses.
More: Trump Mocked as Mike Pence Gets JFK Profile in Courage Award for Defying Him and Certifying 2020 Election
More: “This Is Very Important to the President”: Trump Admin Orders NIH to Study Transgender Regret While Slashing Trans Health Research
For Medicaid, the situation remains patchy. Because it’s state-run, coverage varies widely. Some states provide access, while others have denied it, largely due to high costs. Biden’s plan would have mandated nationwide coverage, streamlining access across all states. Private insurers, meanwhile, remain cautious. States like North Carolina and West Virginia have already removed coverage for state employee benefit plans, citing surging demand and costs.
As for out-of-pocket consumers, prices remain steep. Brand-name drugs such as Ozempic and Mounjaro still cost between $350 and $500 monthly, even after falling from highs exceeding $1,300 earlier this year. The Trump administration’s reversal now leaves millions of Americans uncertain about the future of accessible, government-funded weight-loss medication.
READ NEXT:
- DHS Denies Racial Profiling Amid Growing Backlash Over Immigration Raids
- Paris Hilton candidly reveals the reason behind the ‘NSFW’ title
- Jennifer Garner Honors Ben Affleck With Touching Father’s Day Tribute
- ‘My Dad Doesn’t Use Computers’: Trump Jr. Accidentally Roasts President While Defending TrumpCoin
- Trump Banned from NAACP Convention for First Time in Over a Century — Civil Rights Group Says He’s ‘Dismantling Equality’